免疫系统是保护人体健康的重要防火墙,该系统具有高度的辨别力,能精确识别自己和外来入侵物质,并组织动员免疫细胞对外来病毒病菌实行精确打击,以维持机体的稳定和健康。当人体免疫系统出现问题时,机体则容易被病毒病菌感染而产生各种疾病,甚至肿瘤。研究发现,肿瘤病人的免疫系统处于被抑制状态。因此,尝试恢复免疫系统的功能成为癌症治疗的一个重要切入点。免疫治疗经过多年发展取得了重大的进步。免疫治疗分为两大类,分别是体液免疫和细胞免疫。体液免疫通过抗体调节免疫系统,目前最热门最具代表性的就是针对PD-1靶点的抗体。但该抗体仍然存在几个问题:对于肿瘤只能控制不能治愈;只对部分肿瘤如黑色素瘤、肾癌以及肺癌等有效,能够受益的癌症病人只有约20%。细胞免疫则通过各种免疫细胞直接接触并攻击癌症细胞。国内外临床试验结果均已证实细胞免疫的有效性。
近年来,嵌合抗原受体(CAR)T细胞(以B细胞为作用靶标)对晚期白血病患者的治疗取得了巨大的成功。但是,CAR-T细胞免疫治疗伴随着较为严重的副作用。而通过树突状细胞激活免疫细胞符合机体自然规律,被认为是最好的方法。
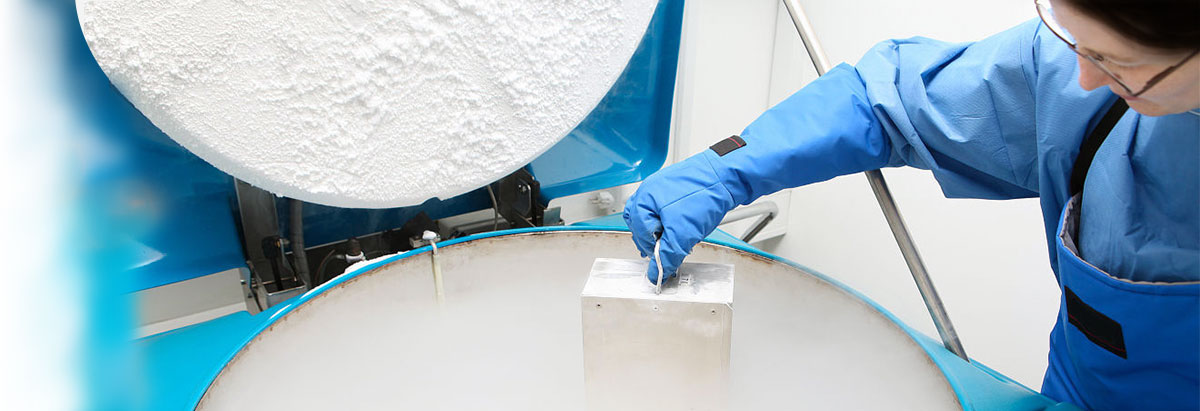
马里兰大学人类病毒学研究所研究团队开发出一种基于树突状细胞(DC)的全新的细胞免疫技术,通过该技术将外周血单个核细胞(PBMC)中的T细胞进行大量扩增并激活成为细胞毒性T淋巴细胞(CTLs),后者具有强大的抗肿瘤作用。该项技术目前已经申请全球专利。DC技术通过多批次、不同类型移植瘤模型被证实是安全且有效的。
DC细胞具有很高的活性,且在长期培养过程中保持这一特性。并且,DC细胞易于进行基因修饰,可以通过改造DC细胞使其能表达不同的癌抗原进而获取特定CTLs细胞。体内外试验均证实DC细胞不仅能够模拟真实的树突状细胞的功能,更重要的是强化其功能,通过其诱导产生的CTLs能够特异性杀伤肿瘤细胞而不损害机体,真正做到安全、有效、可规模化生产。此项技术极有可能为癌症患者的细胞免疫治疗带来新的希望。
The immune system plays an important role in health protection. With its outstanding discrimination performance, the system is able to precisely distinguish between the self and non-self made substances and mobilize the immunocytes in order to combat the targeted foreign viruses and microbes while at the same time maintaining the stability and health of the human body. If the immune system has any problems, the human body will be attacked by the invading viruses and microbes, which can lead to incidences of diseases or even cancers. Studies have shown that the immune systems of cancer patients are generally in an inhibitory state. Therefore, in terms of cancer treatment, it is critical to restore the proper functions of their immune systems.
Immunotherapy has gained a significant development over the years. It can be mainly divided into humoral immunity and cellular immunity. Humoral immunity regulates the immune system through the production of antibodies. Presently, the most popular and representative antibody is the PD-1 antibody. However, there are several problems that are related to this antibody that still remain unsolved. It is only effective in the controlling, but not in the curing of cancers; except for those with melanoma, renal carcinoma and lung cancer—approximately 20% of the total number of cancer patients. However, it shows little treatment efficacy for patients with other types of cancer. Cellular immunity protects the body by activating and stimulating the immunocytes for a straight-pass attack against cancer cells. Both the domestic and foreign clinical trials have demonstrated the effectiveness of cellular immunity.
In recent years, the application of the chimeric antibody receptor-modified (CAR-modified) T-cell therapy (with B-cell as the potential target) to late leukemia patients has achieved spectacular success. However, the CAR-modified T-cell therapy can lead to serious side effects in the patients. As a therapy that binds to the body’s natural laws, the DC-activated cellular immunotherapy is considered as the optimal treatment approach for cancer patients.
The team from the IHV of University of Maryland has developed a new DC-based cellular immunity technology that is able to achieve massive proliferations of T-cells in the peripheral blood mononuclear cells (PBMCs) and transforms them into cytotoxic T-lymphocytes (CTLs), which has a powerful cancer-fighting function. The team has applied for patents for this technology in different countries and regions across the world. By applying the DC technology to a series of tumor transplantation models, both the safety and effectiveness of the DC technology has been demonstrated.
While the DCs remain at a relatively high level of activity in the long-term culturethey are also suitable for gene modification, which enables the production of cancer antigens with different expressions and specific CTLs. Both in-vitro and in-vivo trials have demonstrated the capability of DCs to stimulate, and more importantly, enhance the actual DC functions. The CTLs that are produced based on the induction effect of the DCs specifically kills tumor cells without damaging the body. Hence, it is a safe and effective therapy that is suitable for mass production. The promising technology that is based on cellular immunotherapy is likely to cure cancer patients.